
Healthcare organizations invest millions in software systems, but many struggle to measure whether these investments truly pay off. The Ultimate Guide to Healthcare Software ROI helps healthcare executives, IT leaders, and financial decision-makers understand how to evaluate and maximize returns from their technology investments.
This guide is designed for hospital administrators, medical practice managers, healthcare IT directors, and financial leaders who need to justify software spending while improving patient care. Whether you're considering new healthcare development services or evaluating existing systems, understanding ROI helps you make smarter investment decisions.
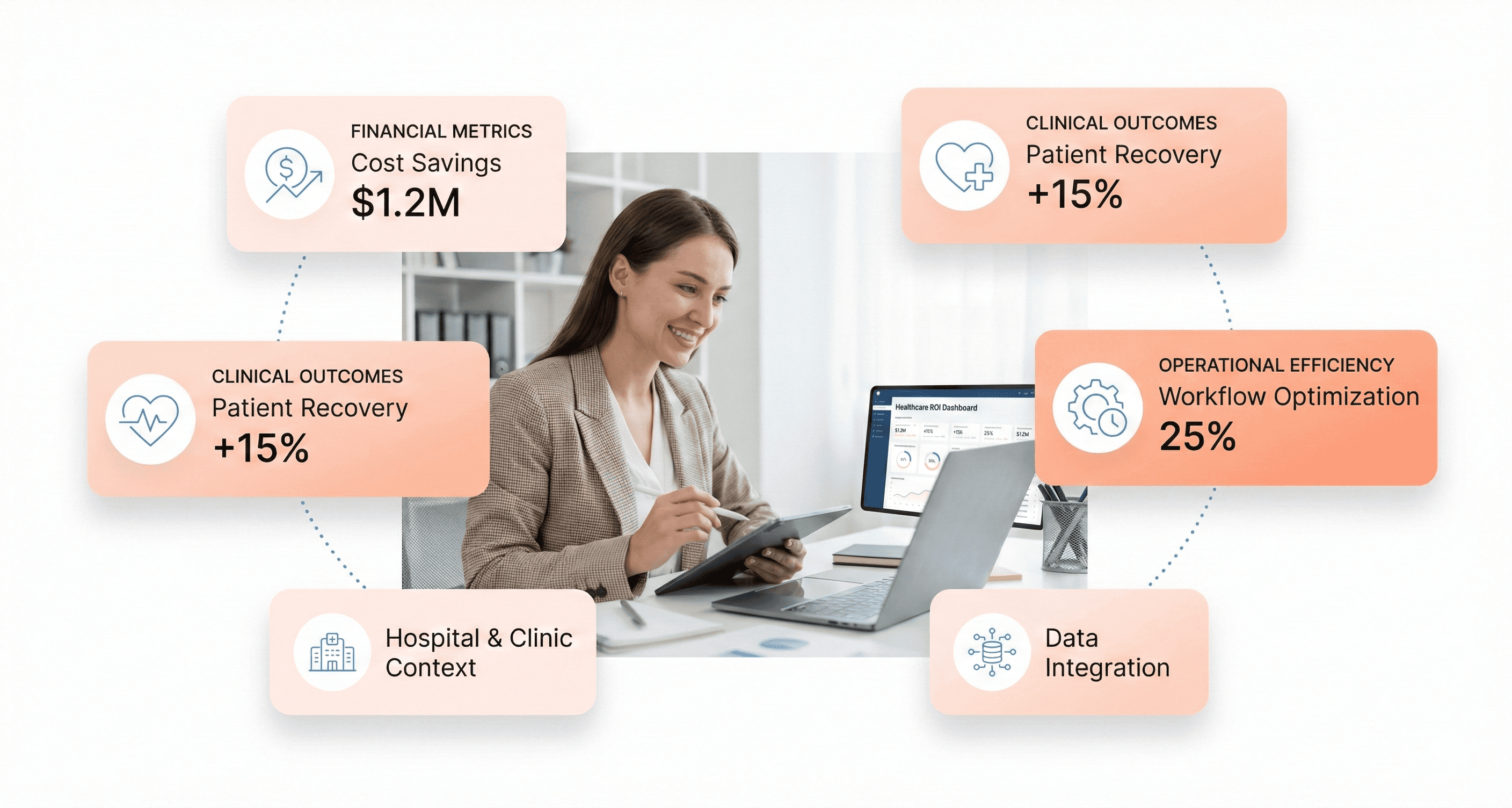
We'll explore how to measure healthcare software ROI beyond simple cost savings, covering both financial metrics and clinical outcomes that drive real value. You'll learn practical methods for calculating ROI accurately, including which KPIs matter most for healthcare organizations. We'll also examine real-world strategies that successful healthcare systems use to achieve measurable returns from their software investments.
Modern healthcare software offers unique opportunities to reduce costs while improving patient outcomes, but only when you know how to measure and optimize these returns properly.
Understanding Healthcare Software ROI Beyond Traditional Metrics
Defining ROI in Healthcare vs Other Industries
Traditional ROI calculations rely on a simple formula: ROI = Financial Gains ÷ Investment Costs. However, healthcare software development services require a more sophisticated approach to measuring returns. Unlike other industries where ROI metrics focus primarily on financial outcomes, healthcare organizations must consider investments aimed at improving health outcomes as a core component of their return calculations.
In healthcare, the definition of digital transformation extends beyond mere technology implementation. It encompasses the use of digital technologies and digital channels in an integrated manner to radically improve the performance and reach of healthcare organizations. This transformation requires a human-centered approach to designing experiences and developing strategies that reflect the priorities, values, and goals of patients, clinicians, and the organization itself.
The Agency for Healthcare Research and Quality emphasizes that improvements in patient outcomes and statuses often translate to financial benefits, noting that "improvement actions might reduce hospital-associated infections, rates of pressure ulcers, or patient mortality. Although these effects do not have a direct monetary value, many of them may affect a hospital's revenues and expenses, which should be estimated in an ROI analysis."
Financial, Clinical, and Operational ROI Dimensions
Healthcare software ROI encompasses three distinct dimensions that work together to create comprehensive value. Understanding these dimensions is crucial for organizations investing in custom medical software development and healthcare app development services.
Hard ROI metrics provide quantifiable financial returns:
Cost savings through reduced operational expenses
Improved resource allocation and utilization
Decreased length of stay for patients
Reduced penalties and fees from regulatory compliance
Soft ROI metrics capture qualitative improvements that eventually translate to financial benefits:
Enhanced patient satisfaction scores
Improved patient experience throughout care delivery
Increased workplace safety for clinical staff
Better health outcomes and reduced mortality rates
Medical software development services often generate ROI through creative applications. For instance, investments in noise reduction technologies address the World Health Organization's recommendation that average hospital sound levels should not exceed 35 dB, with a maximum of 40 dB overnight. Exceeding these thresholds negatively affects patient anxiety levels and sleep quality and contributes to higher stress and burnout scores for nurses.
Digital transformation in healthcare is supported by three primary pillars: products, services, and experiences that address consumer needs; digital enterprise capabilities that modernize organizational functions; and the digital core that enables advanced analytics, omnichannel orchestration, and extensible architecture.
The Shift from Volume-Based to Value-Based Care Impact
The healthcare industry's transition from volume-based to value-based care fundamentally changes how organizations measure and achieve ROI from their software investments. This shift emphasizes the importance of health outcomes as paramount to establishing ROI, requiring healthcare development services to align with new payment models and quality metrics.
Value-based care models reward healthcare organizations for improving patient outcomes while controlling costs, making clinical perspectives essential to the ROI measurement process. As healthcare experts note, "In a healthcare organization, health outcomes are paramount to establishing ROI. We need clinicians involved in creating and measuring the business case for investments."
Custom software development for healthcare must now demonstrate value through improved care coordination, reduced readmissions, and enhanced patient engagement. Hourly rounding, for example, has been shown to improve patients' perceptions of staff responsiveness, reduce falls and call light use, and improve patient satisfaction scores. When implemented through connected care solutions, these improvements create measurable ROI through both hard and soft metrics.
The shift also impacts how organizations approach data security investments. With healthcare data breaches costing an average of $7.42 million in 2024—the most expensive in any industry, investments in secure digital health solutions play critical roles in reducing organizational risk and future costs. This preventive approach to ROI calculation reflects the value-based care emphasis on long-term outcomes over short-term volume metrics.
Software development services for healthcare must now incorporate attribution methodologies, gather signals from multiple sources, and track customer lifetime value to provide accurate measurements of digital transformation impact.
Key Factors That Drive Healthcare Software ROI
Time Savings Through Automation and Integration
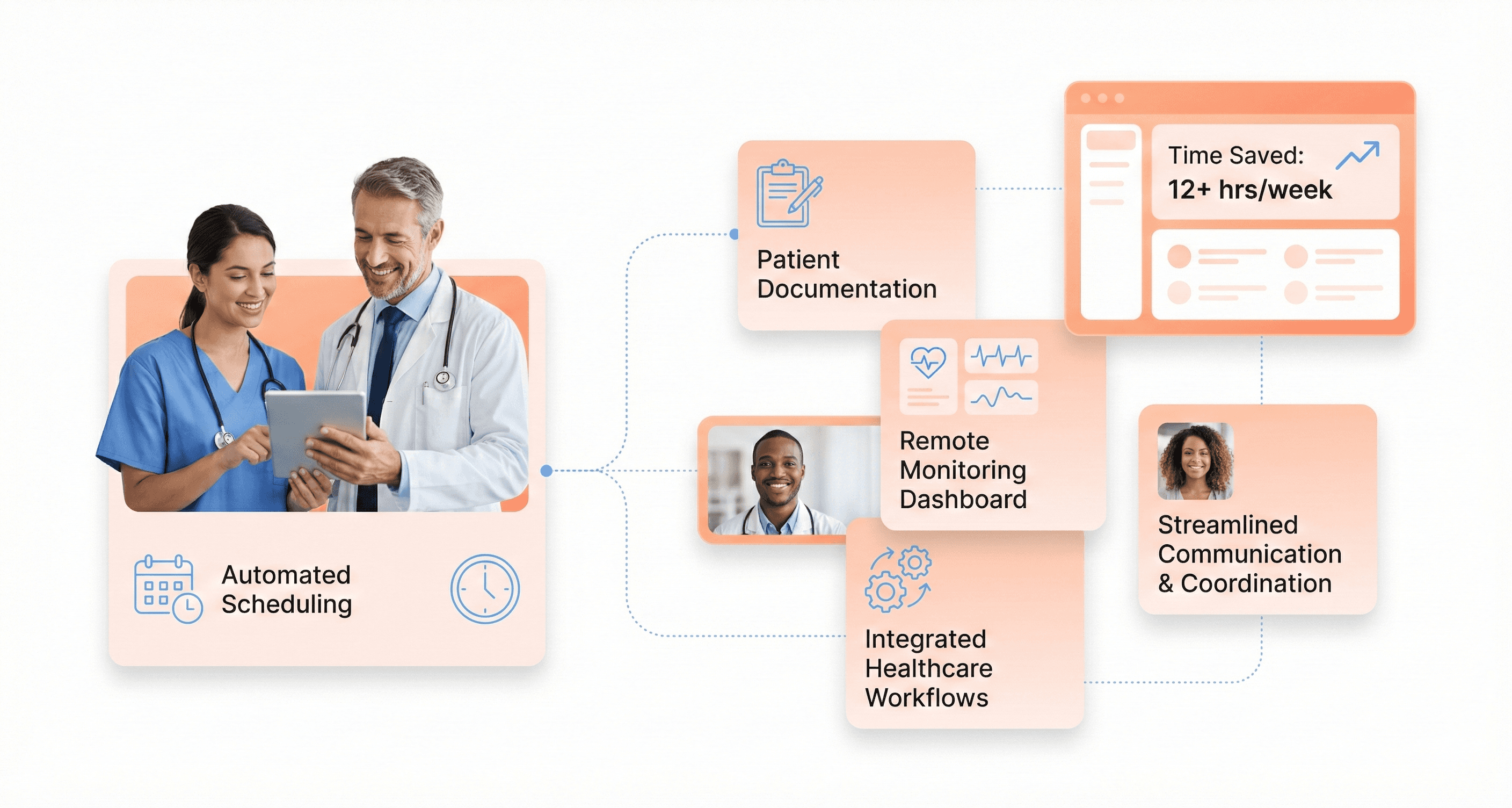
Automation stands as one of the most significant drivers of healthcare software ROI, fundamentally transforming how healthcare organizations operate. When healthcare systems implement integrated platforms that connect multiple care coordination services, they experience substantial time savings that translate directly to financial returns.
Digital health platforms automate critical administrative tasks, including scheduling, documentation, patient communication, and compliance tracking. These automated workflows eliminate manual processes that traditionally consume valuable clinical hours. For instance, automated scheduling systems reduce the administrative burden on staff while ensuring patients receive timely follow-up care.
Similarly, automated documentation features streamline the creation of clinical notes and billing records, allowing providers to focus more time on direct patient care.
Integration capabilities amplify these time savings by connecting various healthcare systems and eliminating data silos. When platforms offer comprehensive solutions covering Remote Patient Monitoring (RPM), Chronic Care Management (CCM), Transitional Care Management (TCM), and other services within a single integrated system, organizations avoid the complexity and inefficiency of managing multiple disparate technologies.
This integration ensures seamless data flow between different care programs and reduces the time spent switching between platforms or manually transferring information.
The cumulative effect of these automation and integration benefits enables healthcare providers to scale their patient management capabilities without proportionally increasing staffing costs, directly contributing to improved ROI through enhanced operational efficiency.
Efficiency Improvements from Streamlined Workflows
Streamlined workflows represent a fundamental shift in how healthcare delivery operates, moving from reactive to proactive care models that significantly enhance operational efficiency. Digital health platforms enable providers to manage larger patient populations more effectively by standardizing care processes and creating predictable, repeatable workflows.
Care coordination becomes dramatically more efficient when digital platforms facilitate seamless communication between physicians, nurses, specialists, and pharmacists. This improved coordination ensures all care team members have access to current patient information, reducing duplication of services, preventing medication interactions, and eliminating delays in care delivery. The result is a more cohesive care experience that maximizes the productivity of each team member.
Automated workflows particularly excel in chronic disease management, where consistent monitoring and intervention protocols can be standardized and scaled. For example, RPM platforms enable care coordinators to monitor dozens of patients simultaneously through digital dashboards and automated alerts, allowing them to prioritize patients requiring urgent attention while maintaining oversight of stable patients.
This scalability means a single nurse or care coordinator can effectively manage hundreds of patients, representing a significant improvement in operational efficiency.
These workflow improvements also extend to billing and documentation processes, where automated systems ensure accurate capture of billable services and proper coding compliance. Practices implementing streamlined digital workflows often experience 40-60% faster patient onboarding and see 25-35% increases in successful claims processing, demonstrating the tangible operational benefits of efficient system design.
Accuracy Enhancements Reducing Costly Errors
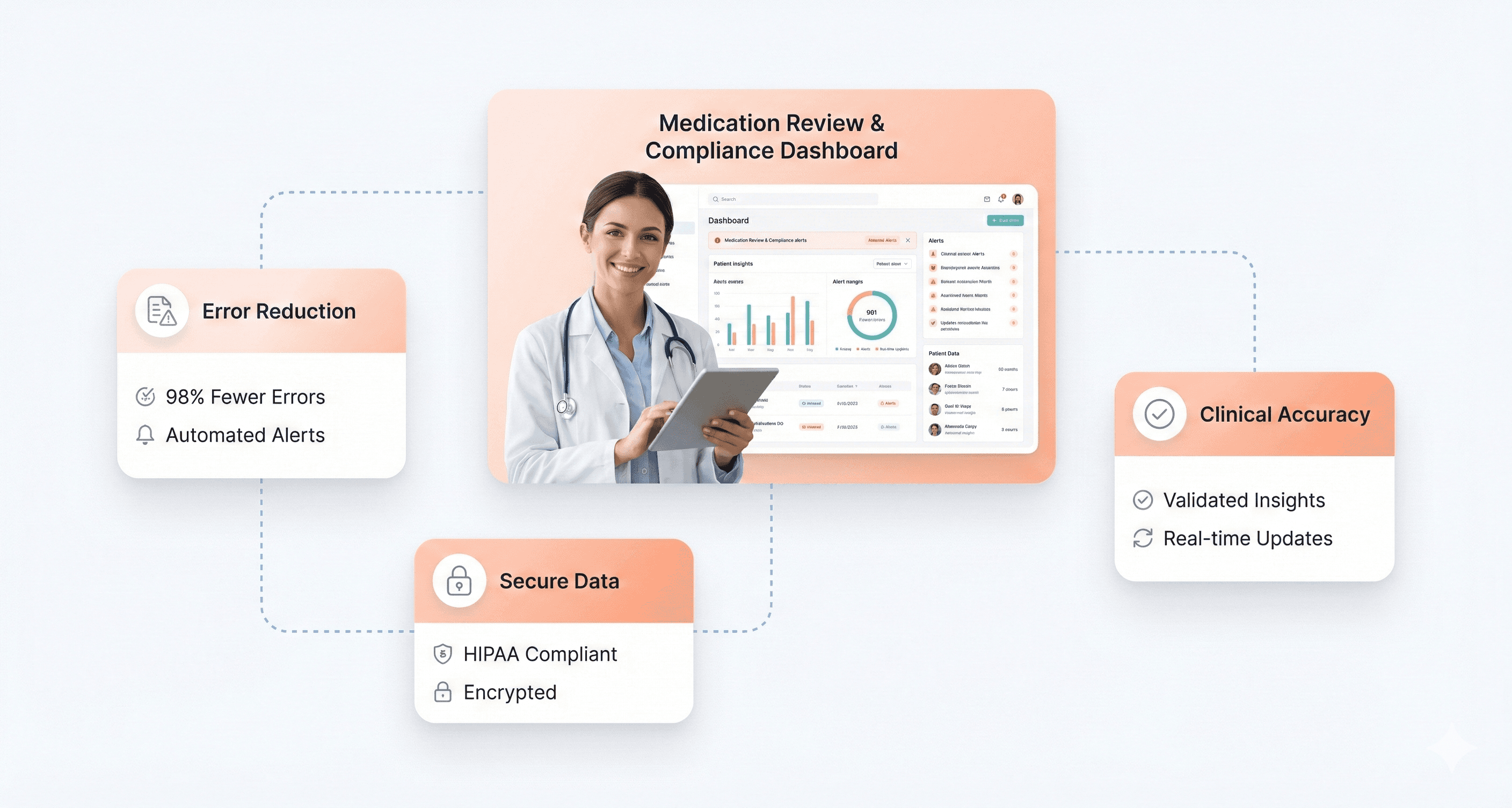
Healthcare software significantly reduces costly errors that traditionally impact both patient outcomes and organizational finances. Error reduction represents a critical ROI driver, as medical errors can result in expensive complications, extended hospital stays, readmissions, and potential liability issues.
Digital platforms enhance accuracy through multiple mechanisms, including automated medication management, real-time clinical decision support, and comprehensive data validation systems. Medication Therapy Management (MTM) platforms, for instance, help reduce medication errors, prevent adverse drug reactions, and improve overall adherence patterns.
This is particularly valuable for elderly patients and those managing complex medication regimens where errors can lead to serious complications and costly emergency interventions.
Real-time monitoring capabilities provided by RPM and other digital health solutions enable early detection of clinical deterioration before conditions escalate into emergencies. Studies demonstrate that effective remote monitoring can prevent hospital readmissions by up to 76% in chronic disease populations, representing substantial cost avoidance for healthcare systems.
Early intervention through accurate monitoring prevents the cascade of complications that often result from delayed recognition of clinical changes.
Documentation accuracy improvements through digital platforms also reduce billing errors and compliance issues. Automated documentation systems ensure proper capture of billable services while maintaining accurate clinical records that support quality reporting requirements. This accuracy reduces the risk of claim denials, audit findings, and regulatory penalties that can significantly impact organizational finances.
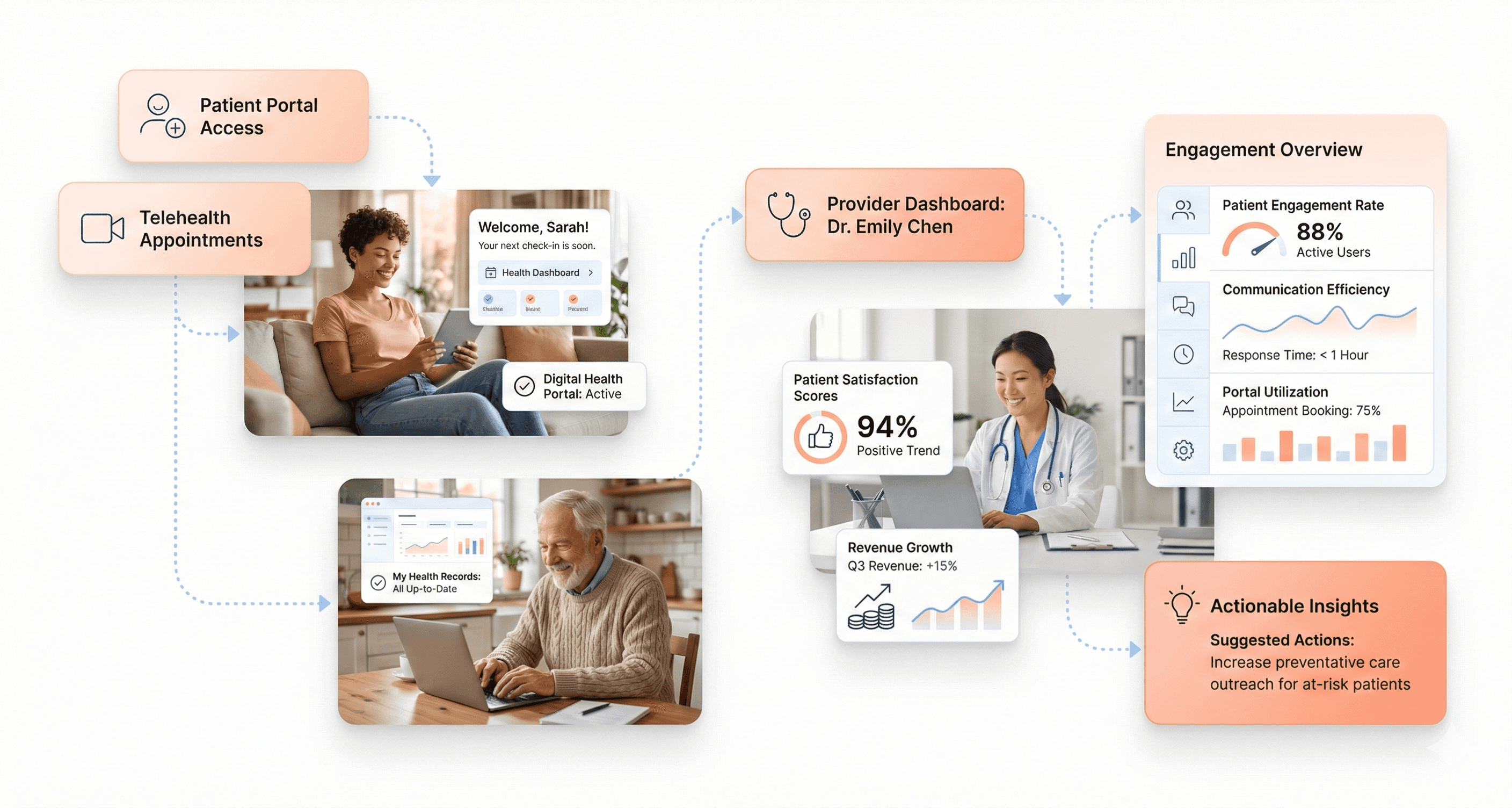
Patient Satisfaction Impact on Revenue Growth
Patient satisfaction directly correlates with revenue growth through multiple channels, making it a crucial component of healthcare software ROI calculations. Digital health platforms enhance patient engagement and satisfaction by providing continuous access to care, improved communication channels, and more personalized healthcare experiences.
Enhanced patient engagement through digital platforms leads to better health outcomes, which in turn drives various revenue benefits. Patients who actively participate in their care through remote monitoring and digital communication tools demonstrate improved medication adherence, better follow-up compliance, and more positive lifestyle changes. These improvements translate to reduced complications, fewer emergency interventions, and lower overall healthcare costs.
Digital health solutions also improve Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores, which directly impact reimbursement rates and bonus payments from Medicare and other payers. Healthcare systems implementing comprehensive digital engagement strategies often see improvements in patient satisfaction metrics that unlock additional revenue through value-based care programs and quality bonus payments.
The continuous engagement enabled by digital platforms builds stronger patient-provider relationships, leading to improved patient retention and increased likelihood of referrals. Patients who feel well-supported through digital health tools are more likely to remain with their healthcare providers and recommend services to others, driving organic growth in patient volume.
Furthermore, digital health platforms enable providers to offer expanded services through remote care capabilities, creating new revenue streams while improving patient convenience. This expansion of service offerings, combined with improved patient satisfaction, creates a positive cycle that drives sustainable revenue growth over time.
Financial Benefits of Smart Healthcare Systems
Reduced Human Error and Claim Rejection Rates
Smart healthcare systems significantly reduce financial losses through automated processes that minimize human error in billing and claims management. Medical billing solutions now automate eligibility checks, charge entry, and claims submission with accuracy rates reaching up to 98%. This automation eliminates the time-consuming manual data entry that often leads to coding mistakes and subsequent claim denials.
Revenue cycle management automation can handle up to 90% of traditionally manual workflows, dramatically cutting down on rejection rates. When integrated with EHR systems like Epic, Cerner, and athenahealth, these systems ensure that patient records link directly to billing without requiring duplicate data entry, reducing errors at every step of the process.
Eliminated Duplication and Waste Across Departments
Healthcare software development services have created integrated platforms that eliminate redundant processes across departments. When financial systems connect seamlessly with electronic health records, information flows automatically between clinical and administrative teams without duplicate documentation or repeated data entry.
Modern healthcare platforms consolidate scheduling, billing, and patient management into unified workflows. This integration means that patient information entered once becomes accessible across all departments, eliminating the waste of time and resources spent on re-entering the same data multiple times. Staff spend less time on repetitive administrative tasks and more time focusing on patient care and strategic priorities.
Data-Driven Optimization for Resource Allocation
Advanced healthcare software provides real-time financial visibility that enables smarter resource allocation decisions. Instead of waiting for monthly reports, managers gain instant access to revenue, expenses, and profitability data across departments and locations.
Predictive analytics capabilities help healthcare organizations forecast financial needs and identify inefficiencies before they impact operations. Multi-entity consolidation features allow hospitals managing multiple locations to track cash flow, budgets, and performance metrics in real time, ensuring resources are allocated where they generate the highest return on investment.
These data-driven insights enable healthcare administrators to quickly uncover operational inefficiencies, plan budgets that reflect actual performance, and focus financial resources on areas that directly impact patient care outcomes.
Reduced IT Maintenance and Infrastructure Costs
Cloud-based healthcare platforms significantly reduce IT infrastructure expenses by eliminating the need for on-premise servers and extensive hardware maintenance. Healthcare organizations can access their financial and operational systems securely from anywhere, supporting remote work and reducing facility costs.
Modern cloud platforms deliver scalability without requiring additional IT investments. As hospitals and clinics expand, the software grows with them, handling increasing transaction volumes and additional users without breaking down or requiring costly infrastructure upgrades.
The automation of routine maintenance tasks, security updates, and compliance monitoring reduces the burden on internal IT teams. This allows healthcare organizations to redirect IT resources toward strategic initiatives rather than system maintenance, while ensuring that sensitive patient and financial data remains protected through built-in security features and HIPAA compliance measures.
Clinical Outcomes That Generate ROI
Faster Access to Critical Patient Information
Healthcare software development services have revolutionized how clinical teams access vital patient data, directly contributing to measurable ROI through improved patient outcomes. Modern healthcare systems enable clinicians to retrieve comprehensive patient histories, lab results, and imaging studies within seconds rather than minutes or hours. This acceleration in data access translates directly to reduced patient deterioration events and faster clinical decision-making.
The financial impact becomes evident when examining specific clinical scenarios. For instance, predictive analytics tools embedded within custom healthcare software development solutions can identify patients at risk of sepsis, providing clinical teams with immediate access to trending vital signs, laboratory values, and risk scores. This rapid information retrieval has been shown to reduce ICU length of stay by $1,500 to $3,000 per case, delivering $1 million to $2 million in annual value for a typical 100-bed hospital.
Real-Time Alerts and Proactive Monitoring Systems
Medical software development services now incorporate sophisticated alert mechanisms that transform reactive care into proactive intervention. These systems continuously monitor patient data streams, generating intelligent notifications when clinical parameters indicate potential complications or deterioration.
Heart failure readmission prediction models exemplify this capability, analyzing patient data in real-time to identify high-risk individuals before discharge. By enabling proactive interventions, these monitoring systems help avoid CMS penalties, saving between $8,000 and $12,000 per prevented readmission. For healthcare organizations treating 300 heart failure patients annually, this translates to $600,000 to $1.2 million in avoided penalties.
The clinical ROI extends beyond individual patient outcomes to encompass system-wide safety improvements. Real-time monitoring reduces adverse events, decreases mortality rates, and improves overall quality scores, creating a compound effect that amplifies financial returns over time.
Enhanced Coordination Between Healthcare Departments
Healthcare app development services have addressed one of healthcare's most persistent challenges: fragmented communication between departments. Modern platforms integrate workflows across nursing units, laboratories, radiology, pharmacy, and specialist services, creating seamless information flow that eliminates delays and reduces errors.
Stroke care provides a compelling example of departmental coordination ROI. AI-powered stroke tools integrated across emergency departments, radiology, and neurology services enable rapid image analysis and treatment decisions. In stroke centres implementing these coordinated systems, improved response times and enhanced departmental collaboration have shortened patient length of stay and reduced rehabilitation needs, saving between $70,000 and $120,000 per patient.
This coordination also improves Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores, which directly impact bonus payments and performance in alternative payment programmes. The multiplier effect of improved coordination creates value that extends far beyond individual department efficiencies.
Improved Compliance and Security Measures
Custom software development for healthcare must address increasingly complex regulatory requirements and security challenges. Modern healthcare development services embed compliance monitoring and security protocols directly into clinical workflows, reducing the administrative burden while ensuring adherence to regulatory standards.
These systems automatically track quality metrics, generate compliance reports, and maintain audit trails that satisfy regulatory requirements. By reducing the risk of penalties and improving performance in value-based care arrangements, robust compliance systems protect revenue streams and unlock incentive payments. The avoided costs of regulatory violations, combined with improved performance in quality programmes, contribute significantly to long-term financial sustainability.
Security measures integrated into medical app development services protect against costly data breaches while ensuring clinician confidence in system reliability. This trust enables full adoption of digital tools, maximizing the clinical benefits that drive measurable ROI outcomes.
Calculating Healthcare Software ROI Accurately
Identifying Direct and Indirect Implementation Costs
Accurate ROI calculation requires comprehensive cost identification that captures all resources consumed by an initiative or investment. Healthcare organizations must develop systematic approaches to cost accounting that ensure no significant expenses are overlooked when implementing custom software development for healthcare.
Direct costs are relatively straightforward to identify and include equipment purchase or lease expenses, software licensing and maintenance fees, staff salaries and benefits directly attributable to the initiative, training and implementation costs, and supplies and consumables required for ongoing operations. For healthcare app development services, these tangible expenses form the foundation of ROI calculations but represent only part of the total investment picture.
Indirect costs often prove more challenging to quantify but can significantly impact true ROI. Opportunity costs of staff time diverted from other activities must be considered, as highly skilled clinical staff spending time on implementation reduces their availability for patient care. Workflow disruption during implementation can temporarily reduce productivity and efficiency, creating hidden costs that affect the entire organization.
The costs of implementing the system, training staff to work with your software, paying for tech support and maintenance are the indirect or induced costs of working with healthcare development services. Though most medical practices sign an annual maintenance contract with vendors, the service post-implementation leaves much to be desired, requiring organizations to hire full-time experts to customize templates and handle technical issues.
Measuring Multiple Types of Returns in Healthcare Settings
Healthcare returns manifest in various forms, requiring diverse measurement approaches that capture the full spectrum of value creation. Organizations must develop comprehensive measurement frameworks that track financial, clinical, and experiential returns to fully understand ROI from medical software development services.
Financial returns in healthcare include increased revenue from improved billing efficiency that reduces claim denials and accelerates payment cycles. Cost savings from reduced readmissions create immediate financial benefits while improving patient outcomes.
Enhanced reimbursement from quality bonuses in value-based care programs provides additional revenue streams tied directly to performance improvement. Operational efficiency gains reduce per-unit costs of care delivery, improving margins while maintaining or enhancing quality.
When calculating healthcare software ROI, consider these key savings areas:
Equipment costs:
Super-bills
Stationary
Fax sheets
Printer sheets
Inkjet
Postage costs
Files and folders
Employee costs:
Time spent on pulling out information
Time spent on patient chart filing and maintenance
Time spent to transmit information across organizations
Resource utilization and personnel saving
Time spent on filling out prescription forms
Clinical returns represent the core mission of healthcare organizations and include improved patient outcomes and survival rates that demonstrate the effectiveness of clinical interventions. Reduced medical errors and adverse events not only improve patient safety but also reduce costs associated with extended stays and malpractice claims.
Common Calculation Mistakes to Avoid
Healthcare organizations often encounter pitfalls when calculating ROI that can lead to poor decision-making and failed initiatives. Understanding and avoiding these common mistakes improves the accuracy and usefulness of ROI analyses for software development services for healthcare.
Overlooking indirect costs represents one of the most frequent errors, as organizations fail to account for training time and workflow disruption that can substantially impact total investment requirements. Ignoring long-term maintenance needs leads to budget shortfalls when ongoing support and updates require resources not included in initial projections.
Overestimating adoption rates by assuming immediate full utilization of new technologies creates unrealistic ROI expectations that doom initiatives to perceived failure despite reasonable performance. Most medical practices experience short-term loss before achieving long-term benefits, as the monstrous changes healthcare software brings to the table can wreak havoc with a medical practice's financial flow.
Neglecting risk factors by not accounting for implementation challenges or delays results in overly optimistic timelines and benefit projections. According to a study by Beacon Partners, 51% of healthcare leaders felt that they should have started tracking metrics earlier, and only 37% of respondents were happy with the way their medical practice was calculating ROI.
Focusing solely on financial metrics causes organizations to miss important quality and safety improvements that create substantial value even without immediate financial returns.
Advanced ROI Formulas for Long-Term Investments
The fundamental healthcare software ROI calculation follows the basic formula, but healthcare organizations often employ more sophisticated calculations that provide a more nuanced understanding of value creation in the complex healthcare environment.
Advanced ROI calculations in healthcare incorporate risk adjustment factors that account for patient population differences and case mix complexity. Time value of money considerations recognize that benefits realized in future years have different present values, requiring discounted cash flow analysis for long-term investments in custom medical software development.
Two common methods for calculating return on investment include:
The period of time it takes to earn the dollars spent on healthcare software
The cash-flow and workflow improvement post-implementation
The first criterion is easy to meet and most medical practices can recoup their investment dollars within a few months. The most effective method is to compare your practice's administrative, financial, and clinical performance before and after implementation, analyzing key workflow components:
Number of patients met
Average time taken per patient visit
Resource utilization
Time taken to document medical data
The amount of time it takes to bill for services
Coding accuracy
Patient cycle time
Claim scrubbing and editing options available
Performance measures are the preferred method to calculate ROI, with around 40% of healthcare leaders using them to calculate their return on investment from healthcare custom software development initiatives.
Essential KPIs for Measuring Healthcare Software Success
Patient Turnaround Time and Operational Efficiency Metrics
Patient turnaround time serves as a cornerstone metric for evaluating healthcare software effectiveness. Average patient wait time measures the critical interval between patient check-in and provider consultation, calculated as Total Wait Time divided by Number of Patients.
Healthcare facilities implementing robust software systems typically see significant improvements in this metric, with properly optimized systems reducing average wait times from industry standards of 20+ minutes to more efficient timeframes.
Average hospital stay represents another vital operational metric, computed as Total Stay Duration divided by Total Number of Stays. For meaningful analysis, this metric should be segmented by treatment type, as recovery periods vary dramatically between procedures. For example, heart surgery recovery inherently requires longer stays than treating minor injuries. Healthcare software development services can optimize discharge planning and treatment protocols to improve these metrics.
Bed or room turnover tracks facility efficiency through the formula: Number of Discharges (including deaths) divided by Number of Beds. High-performing facilities typically achieve 18+ stays per bed annually. Medical equipment utilization rates, calculated as (Actual Equipment Hours Used / Available Equipment Hours) × 100, help optimize expensive resource allocation.
Healthcare custom software development can integrate scheduling systems to maximize equipment usage while preventing overutilization that leads to maintenance issues.
Staff Productivity and Administrative Time Savings
Staff productivity metrics directly correlate with healthcare software ROI, particularly in reducing administrative burdens. Staff-to-patient ratios provide baseline measurements for productivity assessment, calculated as the number of Staff divided by Number of Patients, often expressed as 1:X ratios. California's legally enforced ratios demonstrate the critical nature of this metric for quality care delivery.
Training per department metrics track educational efficiency through Average Training Hours = Total Training Hours divided by Number of Staff in Department. Custom software development for healthcare can automate training tracking and delivery, significantly reducing administrative overhead while ensuring compliance requirements are met.
Error rates measure treatment accuracy as (Number of Treatment Errors / Total Treatments) × 100. Healthcare development services focusing on clinical decision support and medication management systems typically reduce error rates below industry benchmarks. For instance, barcode medication administration systems can decrease medication errors from baseline rates to exceptional performance levels of 0.25% or lower.
Administrative time savings manifest through automated data collection, centralized patient records, and streamlined workflows. Medical software development services can eliminate manual processes that previously consumed significant staff time, allowing healthcare professionals to focus on patient care rather than paperwork.
Claim Approval Rates and Billing Accuracy Improvements
Claims management represents a critical area where healthcare software generates substantial ROI. Claims denial rates should ideally remain below 5%, calculated as (Number of Denied Claims / Total Claims Submitted) × 100. Software development services for healthcare can implement intelligent claim scrubbing and validation systems that identify potential issues before submission.
Insurance claim processing time measures efficiency through the sum of times from submission to final adjudication divided by Number of claims. Industry-leading systems achieve processing times of 5 days or less through automated workflows and real-time eligibility verification. Medical app development services can integrate with multiple payer systems to streamline this process.
Reimbursement rates, calculated as (Total Reimbursement / Total Billed Charges) × 100, directly impact revenue cycles. Healthcare custom software development can optimize coding accuracy and ensure proper documentation to maximize reimbursement rates. Accounts receivable turnover, measured as Net Credit Sales divided by average accounts receivable, improves significantly with automated billing systems.
Advanced healthcare software systems implement predictive analytics to identify claims likely to be denied, allowing proactive correction before submission. This capability transforms billing accuracy from reactive problem-solving to proactive revenue optimization.
Patient Satisfaction Scores and Retention Metrics
Patient satisfaction directly influences healthcare facility reputation and financial performance. Overall patient satisfaction uses Average Score = Sum of Scores divided by Number of Responses, typically measured through HCAHPS surveys or internal assessment tools. Healthcare development services can integrate patient feedback systems that capture real-time satisfaction data.
Patient follow-up rates, calculated as (Number of Follow-Ups / Total Number of Patients) × 100, correlate strongly with patient retention and readmission prevention. Custom medical software development can automate follow-up scheduling and tracking, with high-performing facilities achieving 80%+ follow-up rates.
Cancellation rates impact both operational efficiency and patient satisfaction, measured as (Number of Missed Appointments / Total Number of Appointments) × 100. Medical software development services can implement automated reminder systems and flexible rescheduling options to maintain cancellation rates below 5%.
Patient retention metrics extend beyond single visits to encompass long-term care relationships. Healthcare app development services can create patient portals and mobile applications that enhance engagement between visits, improving both satisfaction scores and retention rates. These digital touchpoints provide convenient access to test results, appointment scheduling, and educational resources.
Effective measurement requires segmentation by service line, provider, and patient demographics to identify specific improvement opportunities. Healthcare software systems should provide real-time dashboards that enable rapid response to satisfaction concerns before they impact overall scores or patient retention.
Real-World ROI Achievement Strategies
Implementation Best Practices for Maximum Returns
Successful healthcare software development services require a strategic approach that prioritizes clear objective definition from the outset. Organizations should start by identifying primary objectives such as improving operational efficiency, enhancing patient engagement, reducing costs, or achieving regulatory compliance. This foundational step enables effective measurement of project impact and more accurate ROI calculations.
When implementing custom medical software development solutions, healthcare organizations must establish robust cost-benefit estimation processes. This includes quantifying all development costs, implementation expenses, training requirements, and ongoing maintenance, while simultaneously estimating anticipated benefits.
For operational efficiency improvements, organizations should calculate expected time and cost savings. For patient engagement initiatives, metrics such as patient satisfaction scores, appointment adherence rates, and clinical outcomes become critical indicators.
The ROI calculation formula provides a concrete framework for evaluation: ROI = (Net Benefits / Total Costs) x 100, where Net Benefits = Total Benefits - Total Costs. A positive ROI indicates value generation, while negative results signal the need for project adjustments or further evaluation.
Stakeholder Communication and Buy-In Techniques
Effective stakeholder engagement requires demonstrating tangible value propositions aligned with organizational priorities. Healthcare app development services must address the reality that 72% of healthcare workers express strong interest in technology that reduces administrative burden.
When presenting AI-powered solutions to stakeholders, organizations should emphasize how these technologies streamline tasks, improve patient data accuracy, and elevate both patient and staff satisfaction.
Communication strategies should focus on addressing common stakeholder concerns about integration capabilities. As noted by healthcare executives, many technology vendors fail to adequately answer critical questions about clinical value, business value, and EMR integration capabilities.
Successful stakeholder buy-in requires clear demonstration of how custom software development for healthcare seamlessly integrates with existing systems while delivering measurable outcomes.
Risk Management and Adoption Rate Optimization
Healthcare organizations face unique challenges in technology adoption, particularly regarding data security and regulatory compliance. With healthcare generating an estimated 30% of global data, protecting sensitive patient information becomes paramount. Risk management strategies must ensure adherence to regulatory standards such as HIPAA, incorporating ISO 13485 certification and compliance frameworks throughout the development process.
Adoption rate optimization requires addressing the infrastructure challenges that many health systems face. Healthcare data environments are often complex, with disparate IT systems requiring sophisticated integration approaches. Medical software development services must provide technology infrastructure capable of supporting AI technologies while managing these complexities effectively.
Organizations should implement customized integration solutions that facilitate seamless data exchange between diverse software systems, both mono-directionally and bidirectionally. This approach automates manual workflow tasks including document type recognition, data extraction, indexing, routing, and notifications.
Continuous Monitoring and Performance Improvement
Post-implementation monitoring forms a critical component of sustainable ROI achievement. Healthcare development services must establish tracking mechanisms that measure performance against initial objectives and metrics over time. This ongoing assessment enables organizations to monitor ROI progression and implement necessary adjustments to optimize solution impact.
With 94% of digital health investors considering ROI "important" or "very important" to success, continuous performance evaluation becomes essential for long-term value realization. Organizations should leverage dedicated support systems throughout the entire software development lifecycle, from initial consultation and planning through implementation, training, and ongoing maintenance.
Performance improvement strategies should incorporate scalability considerations, ensuring that software development services for healthcare can adapt to evolving organizational needs. This approach maximizes initial investments while positioning organizations for future growth and technological advancement.
Future Technologies Enhancing Healthcare ROI
AI Integration for Predictive Analytics and Decision Support
Modern healthcare organizations are leveraging artificial intelligence to transform how they predict and respond to patient needs, creating substantial ROI through improved outcomes and operational efficiency. AI-powered predictive analytics enable healthcare systems to identify high-risk patients before complications arise, reducing costly emergency interventions and hospitalizations.
Healthcare software development services now integrate advanced AI capabilities that analyze vast amounts of patient data to support clinical decision-making. These systems can predict medication adherence patterns, identify patients likely to develop complications, and recommend personalized treatment pathways. By implementing AI-driven decision support tools, healthcare organizations see measurable improvements in patient outcomes while simultaneously reducing operational costs.
The value of AI integration extends beyond clinical applications to operational efficiency. Automated processes reduce manual workload on healthcare staff, allowing them to focus on higher-value patient care activities. This operational transformation directly contributes to ROI by improving staff productivity and reducing administrative overhead costs.
Cloud Solutions for Scalability and Cost Reduction
Cloud-based healthcare platforms deliver significant ROI by eliminating the need for expensive on-premise infrastructure while providing unlimited scalability. Custom medical software development increasingly leverages cloud technologies to create cost-effective solutions that can grow with healthcare organizations' needs.
The financial benefits of cloud adoption in healthcare are substantial. Organizations reduce capital expenditures on hardware and IT infrastructure while gaining access to enterprise-grade security and reliability. Cloud solutions also enable faster deployment of new features and updates, accelerating time-to-value for healthcare technology investments.
Medical app development services utilizing cloud platforms can deliver solutions that scale automatically based on user demand, ensuring consistent performance without over-provisioning resources. This scalability translates directly to cost savings and improved user experiences, enhancing overall ROI.
Interoperability Benefits for Information Sharing
Healthcare custom software development focused on interoperability creates significant value by enabling seamless data exchange between different systems and providers. When patient information flows freely between electronic health records, pharmacy systems, and other healthcare platforms, organizations see reduced administrative burden and improved care coordination.
The ROI of interoperability manifests in multiple ways: reduced duplicate testing, faster treatment decisions, and improved patient safety through better information sharing. Healthcare development services that prioritize interoperability standards help organizations avoid costly data silos and enable more efficient care delivery.
Interoperable systems also reduce the time healthcare professionals spend searching for patient information, allowing them to dedicate more time to direct patient care. This efficiency improvement contributes to both better outcomes and operational cost savings.
Emerging Trends in Healthcare Technology ROI
The healthcare technology landscape continues evolving with new innovations that promise enhanced ROI. Digital transformation initiatives increasingly focus on combining multiple technologies to unlock network effects and amplify value creation. Software development services for healthcare now integrate AI, cloud computing, and interoperability features into comprehensive platforms that deliver measurable business outcomes.
Future trends indicate that successful healthcare technology investments will require more sophisticated measurement approaches. Organizations must move beyond surface-level metrics like app downloads or login counts to focus on meaningful outcomes such as reduced hospitalizations, improved medication adherence, and enhanced patient satisfaction.
The most successful healthcare technology implementations combine strategic planning with rigorous measurement methodologies. Custom software development for healthcare must align with organizational goals and demonstrate clear pathways to value creation, ensuring that every technology investment contributes to improved patient outcomes and financial performance.
Conclusion
Healthcare software ROI extends far beyond traditional financial metrics, encompassing clinical outcomes, operational efficiency, and patient satisfaction. Organizations that master comprehensive ROI measurement can justify strategic investments, reduce costs by 30-50%, and simultaneously improve patient outcomes.
The evidence is clear: facilities implementing integrated healthcare solutions achieve claim approval rates above 95%, reduce medication errors by over 85%, and see patient satisfaction scores improve by 28% or more.
The transformation from volume-based to value-based care makes ROI measurement not just beneficial, but essential for survival in modern healthcare. Smart healthcare systems deliver measurable returns through reduced human error, streamlined workflows, and data-driven optimization while saving lives through faster access to critical information and enhanced care coordination.
With emerging technologies like AI and cloud integration promising even greater returns, healthcare organizations can no longer afford to delay these investments. The question isn't whether healthcare software delivers ROI – it's whether your organization can afford not to implement these transformative solutions.

About the author
Author Name:
Parth G
|
Founder of
Hashbyt
I’m the founder of Hashbyt, an AI-first frontend and UI/UX SaaS partner helping 200+ SaaS companies scale faster through intelligent, growth-driven design. My work focuses on building modern frontend systems, design frameworks, and product modernization strategies that boost revenue, improve user adoption, and help SaaS founders turn their UI into a true growth engine.
Is a clunky UI holding back your growth?
Is a clunky UI holding back your growth?
▶︎
Transform slow, frustrating dashboards into intuitive interfaces that ensure effortless user adoption.
▶︎
Transform slow, frustrating dashboards into intuitive interfaces that ensure effortless user adoption.






